case of a 25 year old female with fever
This is the case of a 25-year-old female, a resident of Nalgonda, and a homemaker, who presented to the outpatient department three days ago with chief complaints of
- Generalised body pains since 9 days
- Bilateral knee ankle, metacarpophalangeal joint pains since 9 days
- Fever since 6 days
- Headache since 6 days
History of presenting Illness
The patient was apparently asymptomatic 9 days ago when she developed generalised body aches which were sudden in onset, continuous, aggravated with the onset of fever and relieved on taking medication.
9 days ago, the patient also had joint pains which were present bilaterally in the knee joints, the metacarpophalangeal joints, and the ankle joints. The Joint pains were of dull character, sudden in onset, continuous, did not cause any functional impairment, and aggravated on the onset of fever.
6 days ago, the patient developed a sudden onset, high-grade fever, associated with chills and rigour. According to the patient, the fever was in the range of 101-104 degrees Fahrenheit as measured on separate occasions, it was continuous with no diurnal variation (the patient denies any fever-free intervals during the day). The fever was relieved with medication.
With the onset of fever 6 days ago, the patient also developed a headache which was sudden in onset, diffuse, throbbing in character, and continuous. It aggravated on rise in body temperature and was relieved on taking medication.
The headache was not associated with nausea, vomiting, retroorbital pain, aura, dizziness, or tinnitus.
At this point, the patient visited an RMP who prescribed her paracetamol for the following symptoms which she consumed three times a day, it provided her with a few intervals of normal body temperature.
The patient was asked to get tested for dengue, the reports were positive for NS1 antigen, hence she came to our outpatient department.
On day 1 of admission (three days ago), the patient developed 6 episodes of vomiting within 12 hours duration. The vomitus was non-projectile, non bile stained. There was absence of blood in the vomitus. There were no aggravated or relieving factors. The vomiting was not associated with neck rigidity, or chest or abdominal pain.
The patient also had four episodes of loose stool which were non-mucoid, non-blood stained. It was not associated with abdominal pain or tennismus.
On admission, Hess test positve
There is an absence of sore throat, facial flushing , Blanchable macular rash(no islands of white in a sea of red)
Absence of neurological symptoms : Seizures , nuchal rigidity , jaundice ,
Past History
The patient is not a known case of Diabetes mellitus type 2, Hypertension, Tuberculosis, Epilepsy, asthma, coronary artery disease
6 Months ago, the patient underwent a cesarian section.
There is no history of blood transfusions in the past.
Family History
There are no similar complaints in the family
Menstrual History - Para 1, Live 1
Age at menarche - 13 years
regular cycles 5/30 days
Not associated with pain or clots
The patient is currently in lactational amenorrhoea
Personal history
Diet: Mixed
Appetite; Reduced since the onset of fever
Sleep: Adequate
Bowel and bladder movements are regular and normal
Addictions: None
Allergies: No known allergies to food or drugs
Community History
The patient suggests the presence of open fields and stored water surrounding her house and the presence of patients diagnosed with dengue fever in her neighbourhood.
She gives a history of visiting a relative's place where there were presence of a large number of mosquitos 1 week before the onset of fever.
Daily routine
- The patient wakes up at 8 am
-consumes breakfast at 9
- Does household chores throughout the day
-lunch at 1 PM
- Dinner at 8 pm
General Examination
The patient was conscious coherent, cooperative, and oriented to time place and person.
The patient is moderately built and moderately nourished
Vitals:
Blood pressure 110/70 mm hg
Temperature: Afebrile
Pulse rate - 73 beats per minute, normal rhythm, volume ,character, no radio radial or radio femoral delay
Respiratory rate 14 per minute
Presence of petechiae on arm - after tourniquet test
Absence of pallor, icterus, cyanosis , clubbing , lymphadenopathy, pedal edema
- conjunctival injection
Systemic examination
Per abdomen
Inspection :
Umbilicus inverted, hernial orifices free, suprapubic transverse scar present, all quadrants move equally with respiration, scaphoid shape.
Palpation :
On superfcial and deep palpation
Tenderness elicited in the right hypochondrium , epigastric region , left hypochondrium and hypogastric region
Abdominal muscle tone normal
No Guarding or rigidity
Hepatomegaly seen
Splenomegaly felt
No palpable masses
Percussion
- Tympanic note heard in all 9 segments of the abdomen
Auscultation
- Bowel sounds heard
Cardiovascular system examination :
S1, S2 Heard
No thrills or murmurs
Apex beat notes in the 5th intercoastal space
Respiratory system examination
Trachea central in position
Bilateral air entry present
Normal vesicular breath sounds were heard bilaterally in all areas
Central nervous system
Higher mental functions normal
Cranial nerve examination: No abnormality detected
Motor system
- Bulk
-Tone : Normal in both upper and lower limbs
- Power- Normal power in both upper and lower limbs
- Reflexes bilateral
Knee jerk +2+2
Ankle jerk +2+2
Biceps reflex +2 +2
Triceps reflex +2 +2
Supinator +1+1
Gait: Normal
Sensory system: Intact
Cerebellum: Normal
Provisional diagnosis: This is a case of a 25-year-old female with high-grade fever associated with chills and rigour, joint pain, Muscle aches, vomiting and loose stools
suggestive of dengue
Investigations
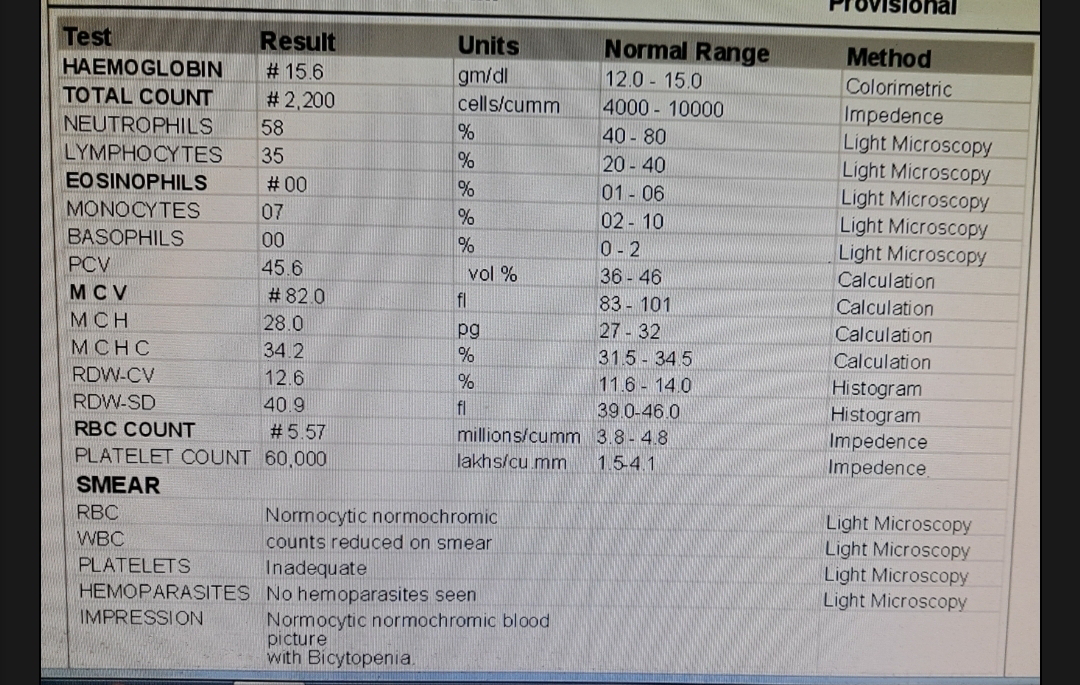
- Complete blood picture -
Packed cell volume and platelet count is normal
There is presence of leukopenia : involving granulocytes : Neutrophils
- Blood sugar estimation
- Electrocardiogram
- Ultrasound abdomen
Management
-Intravenous fluids - Normal saline at 100 ml/hour
- Paracetamol
-Capsule doxycycline 100 mg BD
- Patient education
- Vitals monitoring
- Fever chart ; no saddleback fever
Definitive diagnosis : Dengue fever with thrombocytopenia
Criteria was taken under consideration from
Signs for Probable dengue: Fever + Leukopenia, nausea vomiting arthralgia , myalgia positive torniquet test .
Warning signs of dengue :
Abdominal pain, persistent vomiting, clinical fluid accumulation such as ascites or pleural effusion, mucosal bleeding, lethargy, liver enlargement greater than 2 cm, increase in hematocrit, and thrombocytopenia.-
Schaefer TJ, Panda PK, Wolford RW. Dengue Fever. [Updated 2022 Nov 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430732/




















Comments
Post a Comment