65 year old male with complaints of slurring of speech and inability to swallow since 4 days
*This E-log was created under the guidance of Dr. Chitra Ma'am
A 65-YEAR-OLD MALE PRESENTED WITH CHIEF COMPLAINTS OF SLURRING OF SPEECH AND INABILITY TO SWALLOW FOR THE PAST 4 DAYS.
HISTORY OF PRESENTING ILLNESS
The patient was apparently asymptomatic
20 months ago he was admitted because of?TIA
The patient's family describes it with a deviation of mouth (they are not sure about which side) and weakness of limbs.
1 year back the patient had a history of cerebrovascular accident which he recovered in 1 week where
He was admitted to a hospital for 1 week during which he was diagnosed with Active Pulmonary Koch's, for which he was on ATT for 6 months. His medical records with respect to the cause of admission are not available.
4 days ago, he developed generalized weakness and it worsened the present condition.
The patients family added that he was finding it difficult to walk
On the day of admission, he came with complaints of slurring of speech, drooling of saliva on the right side, and inability to swallow liquid /solid food for the last 4 days, Deviation of tongue present.
HISTORY OF PAST ILLNESS
Known case of
- Pulmonary KOCH's
- h/o CVA
DRUG HISTORY
- ATT for 6 months
PERSONAL HISTORY
- he consumes alcohol 90 ml 3 times a week
- has a history of 30 beedis a day since the last 30 years
- He has a Mixed diet, adequate sleep
- Normal bowel movements
FAMILY HISTORY
- no relevant family history
GENERAL EXAMINATION
- patient is conscious
- slurred speech
- moderately built
- moderately nourished
- absence of pallor, pedal edema, lymphadenopathy, and icterus
VITALS
- BP- 140/90
- Pulse rate - 80 Beats per minute
- Respiratory rate - 18 cycles per minute
- SPO2 - 96 percent
SYSTEMIC EXAMINATION
CARDIOVASCULAR SYSTEM EXAMINATION
- s1, s2 heard
- no murmurs or thrills
RESPIRATORY SYSTEM EXAMINATION
- normal vesicular sounds heard
- bronchial arterial embolization present
EXAMINATION OF THE ABDOMEN
- soft, non-tender
- bowel sounds heard
CENTRAL NERVOUS SYSTEM EXAMINATION
- the patient has dysarthria
- he has a deviation of the mouth to the right side
- inability to swallow
- the tone is increased bilaterally in both upper and lower limbs
- Fasciculations present
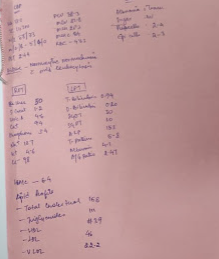
REFLEXES -
RIGHT LEFT
biceps 2+ 2+
triceps 2+ 2+
supinator 2+ 2+
knee jerk - +
abdominal + +
plantar increased increased
INVESTIGATIONS
TREATMENT
DAY 1
- RT feeds with 100 ml Milk 2nd hourly and 100ml water hourly
- INJ PAN 40mg IV /OD
- INJ OPTINEURON 1AMP IN 100 ml NS/IV OVER 30 MINUTES
- PHYSIOTHERAPY OF LEFT UPPER LIMB AND FACE
- TAB. CLOPIDOGREL 75 MG RT/OD
- TAB. ASPIRIN 150MG RT/OD
- TABATORVAS 40 MG RT /OD
- INJ MANNITOL 100 ML 1V
DAY 2
- RT feeds with 100 ml Milk 2nd hourly and 100ml water hourly
- INJ PAN 40mg IV /OD
- INJ OPTINEURON 1AMP IN 100 ml NS/IV OVER 30 MINUTES
- PHYSIOTHERAPY OF LEFT UPPER LIMB AND FACE
- TAB. CLOPIDOGREL 75 MG RT/OD
- TAB. ASPIRIN 150MG RT/OD
- TAB.ATORVAS 40 MG RT /OD
- INJ MANNITOL 100 ML 1V
DAY3
- RT feeds with 100 ml Milk 2nd hourly and 100ml water hourly
- INJ OPTINEURON 1AMP IN 100 ml NS/IV OVER 30 MINUTES
- PHYSIOTHERAPY OF LEFT UPPER LIMB AND FACE
- TAB. CLOPIDOGREL 75 MG RT/OD
- TAB. ASPIRIN 150MG RT/OD
- TAB.ATORVAS 40 MG RT /OD
- INJ MANNITOL 100 ML 1V
- BP MONITORING 4TH HOURLY
DIFFERENTIAL DIAGNOSIS
- ACUTE INFARCT INVOLVING RIGHT TEMPORAL AND PARIETAL LOBES - MCA TERRITORY
- OLD INFARCT involving inferior aspect of the left cerebellar hemisphere
- OLD lacunar infarct in the left thalamus
DISCHARGE SUMMARY
Name of the Treating faculty
DR. MADHUMITHA (INTERN)
DR.CHITRA(INTERN)
DR.DIVYA MAHAPATRA (INTERN)
DR.SWAROOPA (INTERN )
DR.SUBHASHINI(INTERN)
DR.DURGA KRISHNA (PG FIRST YEAR )
DR. AJITH (PG SECOND YEAR )
DR.HAREEN (SENIOR RESIDENT)
DR. RAKESH BISWAS (HEAD OF DEPARTMENT, GENERAL MEDICINE )
DIAGNOSIS
LEFT-SIDED CVA WITH ACUTE INFARCT IN MCA TERRITORY INVOLVING RIGHT TEMPORAL AND PARIETAL LOBE
WITH KNOWN HISTORY OF PULMONARY KOCHS 1.5 YEARS BACK
WITH KNOWN COMPLAINTS OF CVA 1 YEAR BACK AND A HISTORY OF HTN 1 YEAR
CASE HISTORY AND CLINICAL FINDINGS
65Y M CAME TO THE HOSPITAL WITH C/O THE SLURRING OF SPEECH, INABILITY TO SWALLOW LIQUIDS AND SOLIDS SINCE FOUR DAYS THERE WAS ALSO C/O DEVIATION OF MOUTH TO RIGHT SIDE AND INABILITY TO WALK SINCE 4 DAYS.
HE HAS A H/O CVA 1 YEAR BACK WHICH RESOLVED IN 1 WEEK DURING WHICH HE WAS DIAGNOSED WITH ACTIVE PULMONARY KOCHS FOR WHICH HE TOOK 6 MONTHS, AS MENTIONED BY HIS ATTENDANTS
THE PATIENT WAS UNABLE TO WALK WITHOUT SUPPORT AND WAS FROTH SPILLAGE FROM THE RIGHT SIDE OF THE MOUTH
ALCOHOL CONSUMPTION 90 ML 3 TIMES A WEEK
30 BEEDIS SINCE THE LST 30 YEARS
GENERAL EXAMINATION - PATIENT IS CONSCIOUS WITH SLURRED SPEECH, MODERATELY BUILT, AND MODERATELY NOURISHED. NO PALLOR ICTERUS, CYANOSIS, LYMPHADENOPATHY, EDEMA
BP-110/70MMHG
PR - 80 BPM
RR- 18 CPM
SPO2- 96 PERCENT
RESPIRATORY SYSTEM - NVBS HEARD, BAE PRESENT
CVS- S1, S2 HEARD, NO MURMURS OR THRILLS
CNS -
PATIENT HAS DYSARTHRIA
DEVIATION OF MOUTH TO THE RIGHT SIDE, INABILITY TO SWALLOW
TONE IS INCREASED BILATERALLY IN UPPER AND LOWER LIMBS
REFLEXES IN RT LT
B2+2+
T2+2+
S2+2+
K-+
A++
P B/L INCREASED
FASCICULATIONS PRESENT
INVESTIGATIONS -
- ACUTE INFARCT INVOLVING RIGHT TEMPORAL AND PARIETAL LOBES MCA TERRITORY
- OLD INFARCT INVOLVING INFERIOR ASPECT OF LEFT CEREBELLAR HEMISPHERE
- OLD LACUNAR INFARCT IN LEFT THALAMUS
TREATMENT GIVEN
THIS IS A CASE OF A 65-YEAR-OLD MALE WITH ACUTE ISCHEMIC STROKE IN THE MCA TERRITORY INVOLVING THE RIGHT TEMPORAL AND PARIETAL LOBE
THE PATIENT WAS ADMITTED AND RYLES TUBE WAS INSERTED FOR FEEDING AND TAB ASPIRIN, CLOPIDOGREL, AND ATORVASTATIN WERE ADDED AS SECONDARY THROMBOEMBOLIC PROPHYLAXIS. THE CONDITION OF THE PATIENT AND RECOVERY WAS CLEARLY EXPLAINED TO THE ATTENDEES AND ADVICE FOR DISCHARGE AND ASKED TO CONTINUE THE SAME TREATMENT AT HOME.
TREATMENT
DAY 1
- RT feeds with 100 ml Milk 2nd hourly and 100ml water hourly
- INJ PAN 40mg IV /OD
- INJ OPTINEURON 1AMP IN 100 ml NS/IV OVER 30 MINUTES
- PHYSIOTHERAPY OF LEFT UPPER LIMB AND FACE
- TAB. CLOPIDOGREL 75 MG RT/OD
- TAB. ASPIRIN 150MG RT/OD
- TABATORVAS 40 MG RT /OD
- INJ MANNITOL 100 ML 1V
DAY 2
- RT feeds with 100 ml Milk 2nd hourly and 100ml water hourly
- INJ PAN 40mg IV /OD
- INJ OPTINEURON 1AMP IN 100 ml NS/IV OVER 30 MINUTES
- PHYSIOTHERAPY OF LEFT UPPER LIMB AND FACE
- TAB. CLOPIDOGREL 75 MG RT/OD
- TAB. ASPIRIN 150MG RT/OD
- TAB.ATORVAS 40 MG RT /OD
- INJ MANNITOL 100 ML 1V
DAY3
- RT feeds with 100 ml Milk 2nd hourly and 100ml water hourly
- INJ OPTINEURON 1AMP IN 100 ml NS/IV OVER 30 MINUTES
- PHYSIOTHERAPY OF LEFT UPPER LIMB AND FACE
- TAB. CLOPIDOGREL 75 MG RT/OD
- TAB. ASPIRIN 150MG RT/OD
- TAB.ATORVAS 40 MG RT /OD
- INJ MANNITOL 100 ML 1V
- BP MONITORING 4TH HOURLY
ADVICE AT DISCHARGE
- TAB ASPIRIN 150 MG/RT/OD AT 2 P.M.
- TAB CLOPIDOGREL RT/OD AT 9 P.M.
- TAB ATORVAS 40 MG /RT/OD AT 9 PM
- TAB. INCOVIT RT/OD
- PHYSIOTHERAPY OF LEFT UPPER LIMB








Comments
Post a Comment