case of a 34 year old male
This is the case of a 34 year old male , autodeiver by occupation , resident of West Bengal who presented to the hospital with chief complaints of
- pus coming out from behind the upper left last molar since 1 month
History of Presenting Illness
The patient was apparently asymptomatic 1 and a half year ago when he developed pain in the left jaw . The pain was sudden onset , continuous , dull aching in character, present at the point in the upper left jaw behind the last molar. The patient describes the pain with heaviness of the jaw. The patient visited a doctor who prescribed him pain killers. The pain subsided but reappeared after 1 week of using medication. No history of trauma
In the next month , the patient experienced bursting of a swelling in the mouth in the left upper jaw behind the last molar. This resolved the pain completely.
There was a sudden onset of pus discharged from behind that point . The pus was yellow in color, thick in consistency,serous, appreaded every 1- 2 hours on its own, and also appeared when the patient touched his tongue to the site. The pus was not blood stained.
The patient visited our hospital and was reffered to the dental department where he underwent surgery.
For 1 year the patient had no symptoms,
At present , the patient has a reappearance of pus discharge from the same site with same characteristics. The patient also complains of hearing loss in the left ear, which was insidious in onset, gradually progressive. The patient has difficulty hearing in left ear since 1 year . There is absence of tinnitus, aural fullness, pain or discharge from the ear.
For the past 1 month, the patient has had a rise in blood sugars which were detected but no treatment was taken .
Past History
The patient has a left eye corneal opacity since childhood.
Since then the patient has hazy vision in the left eye.
There is history of dental surgery
Not a known case of hypertension , TB , Epilepsy.
Family history
No similar complaints in the family.
Personal History
Diet : Mixed
Appetite : Normal
Bowel and bladder movements: Normal
Sleep adequate
Addictions :
Occasional consumption
of alcohol. Stopped in 2013.
History of smoking from 2008 to 2013 - 3 to 4 cigarettes a day .
Chewing of tobacco from 2010 to 2021
3 to 4 a day .
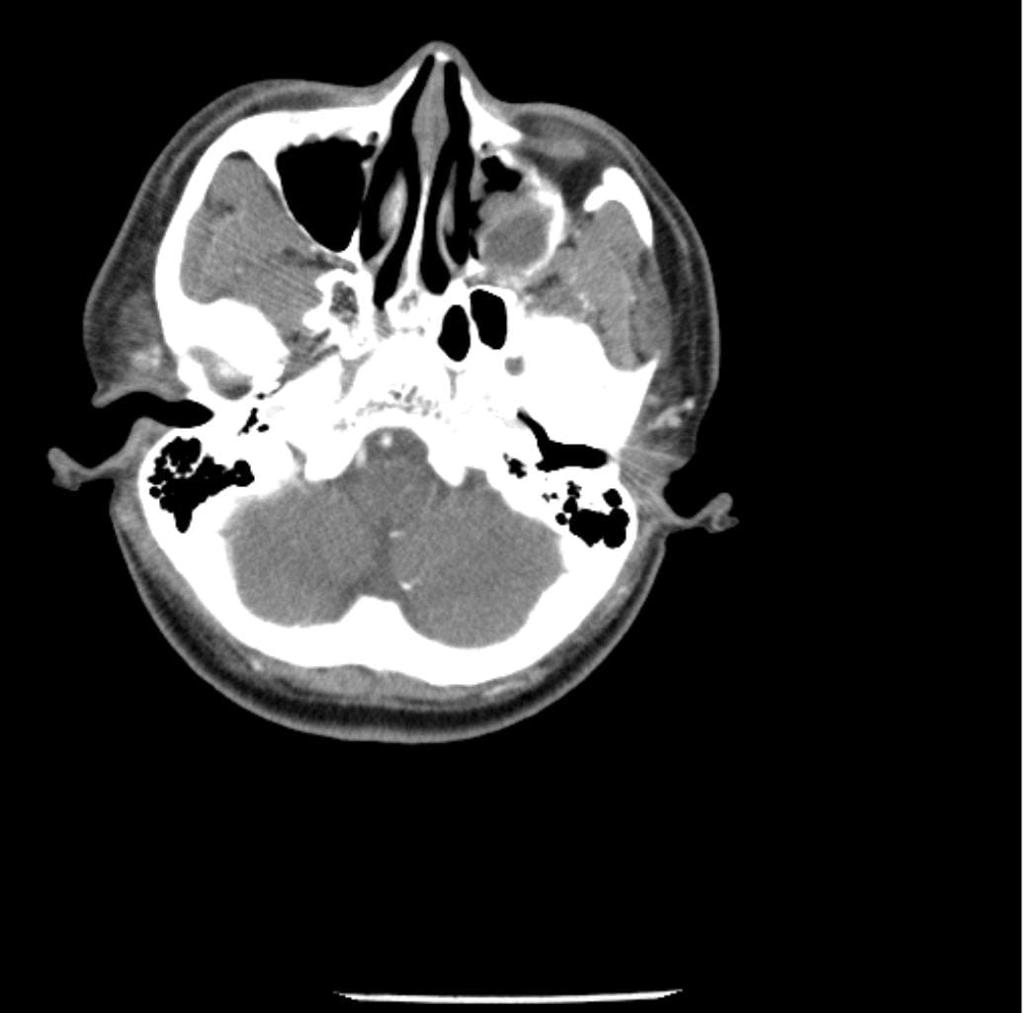
Previous reports and admission:
Examination of Ear Nose , Throat
No paranasal sinus tenderness
Tonsills not visualised
Examination of the eyes
Left eye : hand movements perceived, opacification seen .
Bilaterally : pupillary light reflex, accommodation reflex normal
Provisional Diagnosis?
recurrent periodontal fistula
With Diabeties mellitus type 2





















Comments
Post a Comment